Body mass index is a measurement of your weight relative to your height calculated in order to assess body fat. Adults who have a BMI of 18.5 or lower are considered underweight, over 25 is considered overweight and over 30 is considered obese. BMI is in almost every health screen assessment used by health professionals, sport coaches and trainers. Some insurance companies are even using it as a determinant of your coverage rate.
However, BMI’s validity to assess health, or even obesity, is questionable. Although it’s known as a measure of body fat, it was not created for that purpose. The BMI was created in 1830 by Lambert Quetelet, an astronomer and mathematician but not a medical doctor. Quetelet came up with the formula of a person’s weight in kilograms divided by their height in meters squared to 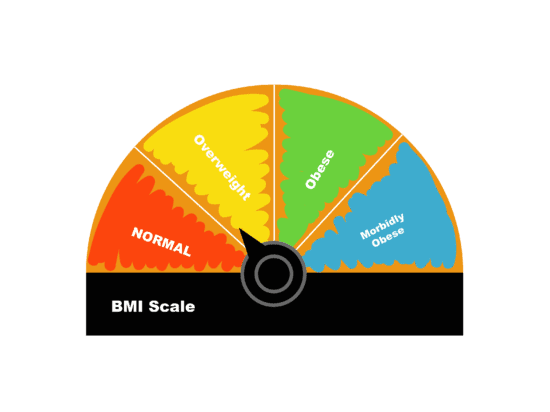 quantify the average growth curve of our height and weight. It is now 2017, and we are still using this formula as a way to screen and measure obesity, not growth.
quantify the average growth curve of our height and weight. It is now 2017, and we are still using this formula as a way to screen and measure obesity, not growth.
The World Health Organization has standardized obesity as having body fat comprise above 25 per cent of your weight for men and 35 per cent for women. However, weight is not always an accurate indication of one’s body fat percentage or even one’s health.
The number on a bathroom scale tells the weight of your total body mass — including the weight of your bones, muscles, water, tissues and organs, in addition to fat. It’s not uncommon for muscular athletes and even average, recreational weight lifters to be considered obese on the BMI scale, despite having a lower body fat percentage than someone who has a lower BMI.
Weight also differs between sexes and ethnicities, not to mention that a person’s weight can fluctuate within a day due to gain and loss of water. One study comparing BMI results across different sexes and ethnic groups found that, in comparison to body fat measuring devices, the BMI gave false positives up to 50 per cent of the time — meaning half of those labelled as “obese” based on BMI were actually not obese.
Despite these issues, BMI is still viewed as the most common test to see whether someone is at a healthy weight. From a health standpoint, having a high bone and muscle mass is protective to your health, but having a high percentage of fat can negatively affect your health. A person with low bone and muscle mass with a high fat percentage can be at risk for heart disease and diabetes but have a “healthy” BMI.
This is apparent in older adults who go through muscle and bone loss in response to aging, which can be a valid indicator of mortality risk. Even, surprisingly, those in the “overweight” category have been found to live longer than those in the “healthy” weight category.
Frankly, your BMI is just an arbitrary number that doesn’t give an accurate reading of fat mass and tells you nothing about health. Even government health websites, such as Canada’s Diabetes Association, lay out the serious flaws with the scale and deem it inappropriate to use to measure athletes, children and older adults. Yet it is still being used and taught as a vital health-screening tool. Why? Maybe because it is easy to do, it has been used since 1830 or it requires no fancy equipment.
Knowing that BMI is essentially pointless and that other devices have a high degree of error, can we just ditch the scale and measure health in other ways? Making changes such as reducing body fat through a caloric deficit diet and building muscle through strength training improve both appearance and health in a drastic way, yet sometimes these benefits are not revealed on the BMI scale.
Body weight or body fat is just one measurement of dozens that can give some clue as to whether or not someone is at risk of chronic disease. Throw that scale away and start living healthier.
—
Florence Scheepers
Graphic: Lesia Karalash / Graphics Editor
Leave a Reply